The here and now
Access to emergency services
Outcome one // Effectiveness indicator
The Australasian College for Emergency Medicine (ACEM) developed the Australasian Triage Scale (ATS) to ensure that patients presenting to Emergency Departments (EDs) are medically assessed, prioritised according to their clinical urgency and treated in a timely manner.
This performance indicator measures the percentage of patients being assessed and treated within the required ATS timeframes. This provides an overall indication of the effectiveness of WA’s EDs, which can assist in driving improvements in patient access to emergency care.
ACEM targets for each ATS targets are outlined below:
| Triage category | Treatment acuity (maximum waiting time for medical assessment and treatment) | Target (threshold) |
| 1 | Immediate ≤ 2 minutes | 100% |
| 2 | ≤ 10 minutes | 80% |
| 3 | ≤ 30 minutes | 75% |
| 4 | ≤ 60 minutes | 70% |
| 5 | ≤ 120 minutes | 70% |
These recommended times and categories are used both locally by the WA Department of Health and nationally by the Department of Health and Ageing, and the Australian Institute of Health and Welfare.
Triage category 1
| Year | Target | Actual | |
|---|---|---|---|
| Years 2024-25 | Target 100% | Actual 99.9% |
|
| Years 2023-24 | Target | Actual 98.3% |
|
| Years 2022-23 | Target | Actual 99.0% |
|
| Years 2021-22 | Target | Actual 99.6% |
|
Triage category 2
| Year | Target | Actual | |
|---|---|---|---|
| Years 2024-25 | Target 80.0% | Actual 61.3% |
|
| Years 2023-24 | Target | Actual 71.7% |
|
| Years 2022-23 | Target | Actual 69.0% |
|
| Years 2021-22 | Target | Actual 68.0% |
|
Triage category 3
| Year | Target | Actual | |
|---|---|---|---|
| Years 2024-25 | Target 75.0% | Actual 13.1% |
|
| Years 2023-24 | Target | Actual 18.8% |
|
| Years 2022-23 | Target | Actual 17.1% |
|
| Years 2021-22 | Target | Actual 18.8% |
|
Triage category 4
| Year | Target | Actual | |
|---|---|---|---|
| Years 2024-25 | Target 70.0% | Actual 28.9% |
|
| Years 2023-24 | Target | Actual 37.3% |
|
| Years 2022-23 | Target | Actual 38.7% |
|
| Years 2021-22 | Target | Actual 41.5% |
|
Triage category 5
| Year | Target | Actual | |
|---|---|---|---|
| Years 2024-25 | Target 70.0% | Actual 64.6% |
|
| Years 2023-24 | Target | Actual 72.4% |
|
| Years 2022-23 | Target | Actual 73.3% |
|
| Years 2021-22 | Target | Actual 78.1% |
|
Period: 2021-22 to 2024-25 financial years
Contributing sites: Armadale/Kelmscott District Memorial Hospital, Royal Perth Hospital, St John of God Midland Public Hospital
Data source: Emergency Department Data Collection
Performance against ATS category 2-5 targets deteriorated in 2024-25, with sites experiencing ongoing demand pressures, both on their Emergency Departments as well as inpatient beds.
EMHS experienced continued changes in the complexity and acuity of patient presentations, with the volume of triage 1 and 2 presentations increasing in 2024/25.
To address growing demand and complexity, initiatives are being rolled out across EMHS sites, these include:
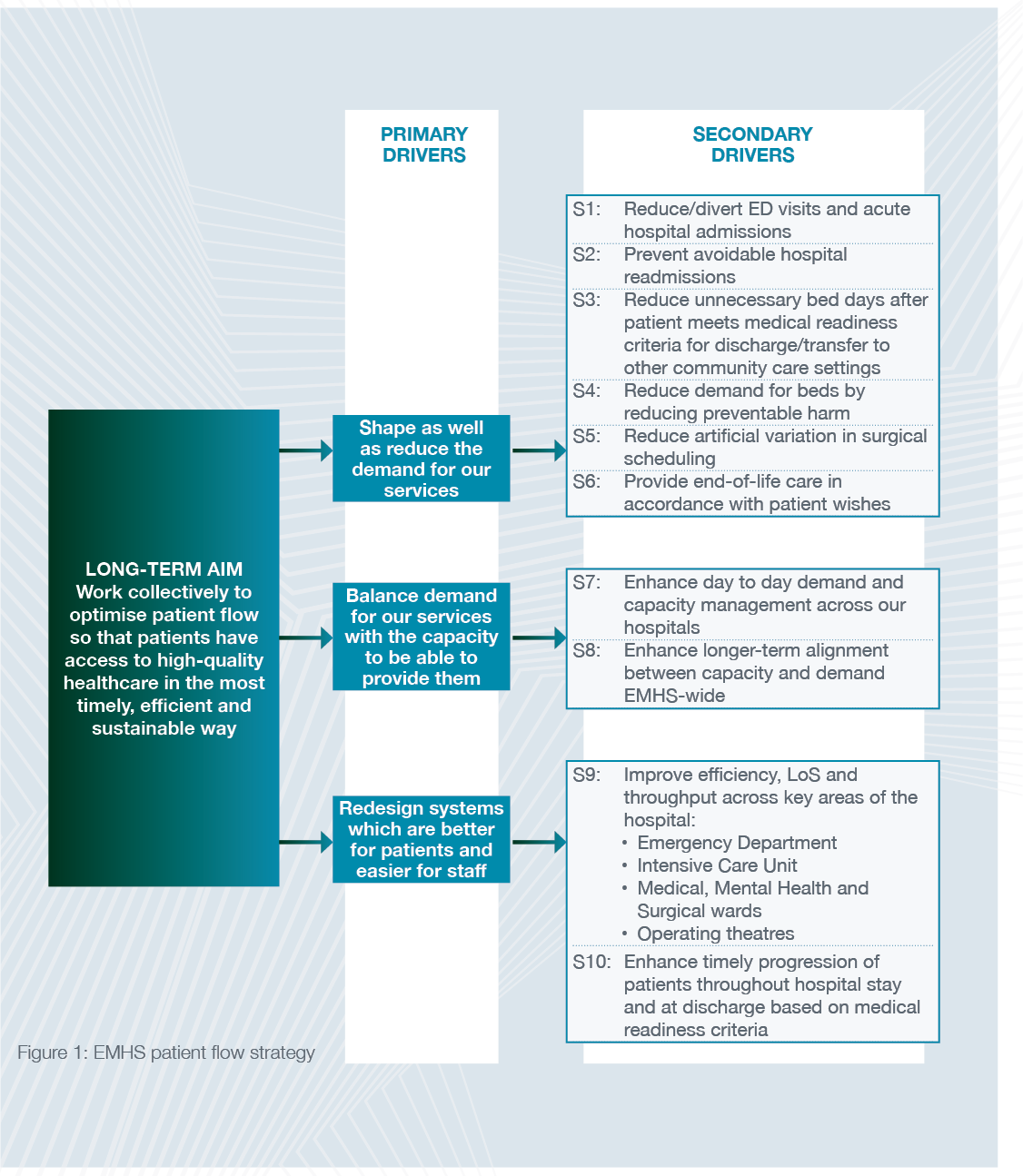
Launch of EMHS patient flow strategy
In December 2024, EMHS launched the Strategic Approach for Optimising Patient Flow. Primary drivers identified to improve access and reduce ED waiting times include:
- shape as well as reduce the demand for our services, so that we can provide care when it is needed most
- optimise the capacity of our services to effectively meet evolving demand
- redesign systems that are better suited to meet the needs of patients and are easier for staff to navigate.
Demand and capacity optimisation program
The Department of Health’s Demand and Capacity Optimisation and the Ambulance Ramping Strategy launched in early 2025 has several immediate priorities to improve patient flow at a system level. These priorities include:
- refining State Health Operations Centre (SHOC) functions, finalising ED benchmarking and cross system Black, Red, Amber, Green (BRAG) (capacity status indicator system), to allow for the rapid identification of capacity related pressure which then can be used to inform demand allocation at the system-wide level
- optimising State-funded aged care beds and services (including Time to Think, in-home transitional care placement, older adult mental health beds) to maintain hospital bed capacity for patients who are acutely unwell
- expansion of Home Hospital to provide care for patients in an environment which suits them the most
- Ambulance Mental Health Co-Response expansion.
Expansion of ambulatory care
The ambulatory units across EMHS continue to provide important pathways to improve flow from EDs. These units divert suitable patients from the ED for same day assessment and management.
To continue to expand the impact of Ambulatory Care Units in 2024-25 we have:
- extended Ambulatory Unit operations from 5 to 7 days per week at Royal Perth Hospital (RPH) during periods of pressure
- from April 2025, the St John of God Midland Public Hospital Ambulatory Care Unit opened 7 days a week to respond to increased demand. Extending the Ambulatory Care Unit will improve flow and reduce ED waiting times on the weekend.
Home Hospital capacity
Home Hospital capacity was launched in 2024 for Royal Perth Hospital (RPH) and commissioned in mid-2025 for Armadale Health Service (AHS). Home Hospital will scale up to 70 beds for EMHS patients by the end of 2025. Home Hospital allows patients to safely return to their normal place of residence and receive the right care at the right place and create capacity for patients requiring acute care in a hospital setting.
Extension of operating hours of the transit lounge at RPH and discharge lounge at AHS
Transit and discharge lounges allows beds to be available earlier in the day (with a focus on moving patients before 10am), reducing access block when transferring patients from ED to the wards. RPH and AHS have extended the hours of the transit lounge to the weekends and evenings to improve patient flow and reduce access block, during periods of pressure.
Creation of Patient Access Division at Royal Perth Bentley Group (RPBG)
The creation of a Patient Access Division in August 2024 established dedicated resources to reduce access block and improve patient care on the emergency pathway. Since the creation achievements to date include:
- reintroduction of senior nursing roles to the Operations Hub
- increased Transit Lounge utilisation
- improvement in the timeliness of inter-hospital transfers
- higher proportion of discharges before noon.
Improving paediatric services at Armadale Health Service (AHS)
To improve the care provided for paediatric patients, AHS is developing a plan to trial a new Paediatric Clinical Decision Unit (CDU), launching in winter 2025. The Paediatric CDU will provide a safe and child friendly environment within the Paediatric Ward, and allow rapid access to specialty paediatric care for children arriving in ED.
Introduction of SPEAR (Senior Practitioner Early Assessment and Review) at St John of God Midland Public Hospital (SJGMPH)
In 2024, SJGMPH, began a reconfiguration in the post-triage space to stream patients into ‘vertical’ or ‘horizontal’ streams, with vertical patients placed in chairs instead of cubicles and stretchers. Building on this, in 2025 SJGMPH introduced the Senior Practitioner Early Assessment and Review (SPEAR) service which involves the improved utilisation of general practitioners and nurse practitioners to treat ATS 4 and 5 patients in a dedicated space adjacent to the ED wait room. The additional clinical staffing capacity reduces waiting times and improves access to care.
Expansion of hospital capacity at SJGMPH
The State Government has previously committed to purchasing the private patient facility within the SJGMPH site to increase public hospital inpatient capacity by 60 beds and three operating theatres from August 2026. The additional inpatient capacity will enhance timely access to beds for patients requiring acute care, and improve flow and waiting times in ED.
New patient record system now online across East
The rollout of digital medical records across all EMHS sites was successfully completed this year, as we modernise our record keeping and availability and look to even further capabilities in the future.
Royal Perth Hospital (RPH) and Bentley Health Service (BHS), along with their corresponding community mental health services, made the big transition from paper to digital records in May and March respectively.
This follows Armadale Health Service and Kalamunda Hospital introducing the change the year before.
The Digital Medical Records (DMR) system at EMHS is part of a statewide implementation across the public health system. It enables clinicians working in the public sector to simultaneously access patient records, improves record tracking and reduces physical storage needs.
By June 2025, a total of 734,793 digital records had been created at RPH and BHS since the DMR system came online at these sites. It is being used by an average 2300 staff members a day across these services.
The DMR system is part of stage one of the WA Health Electronic Medical Record Program aligned with the broader WA Health Digital Strategy 2020-2030.
Its successful implementation across EMHS has us well placed for the adoption of an even more sophisticated electronic medical record system with increased capabilities in the future.


